A Clinical, Epidemiological, and Mental Health Overview
Nipah Virus: An Overlooked but Extremely Dangerous Infection A Clinical, Epidemiological, and Mental Health Overview
The modern world has repeatedly faced the emergence of infectious diseases that challenge healthcare systems and disrupt normal social functioning. While some outbreaks receive immediate global attention, others remain largely unrecognized despite their devastating outcomes. Among these lesser-known yet highly lethal infections is the Nipah virus (NiV).
Based on professional clinical exposure, academic engagement, and continuous evaluation of international research findings, Nipah virus must be regarded as a medical emergency with profound neurological and psychological consequences. Its danger lies not only in its high fatality rate but also in the absence of targeted treatment, lack of vaccination, and its capacity to spread across species barriers. These factors collectively make Nipah virus one of the most concerning emerging infections of recent decades.
What Is Nipah Virus?

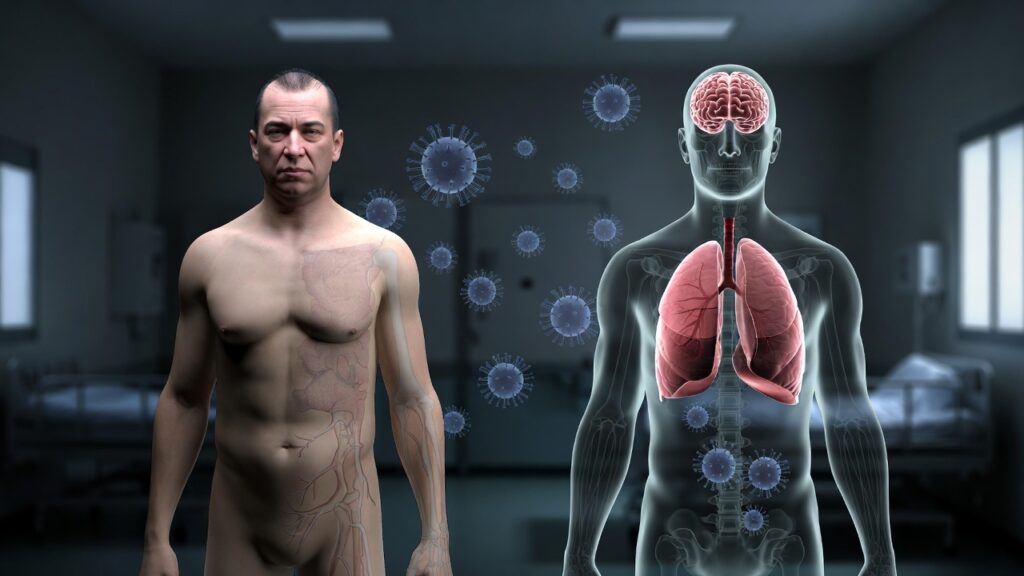
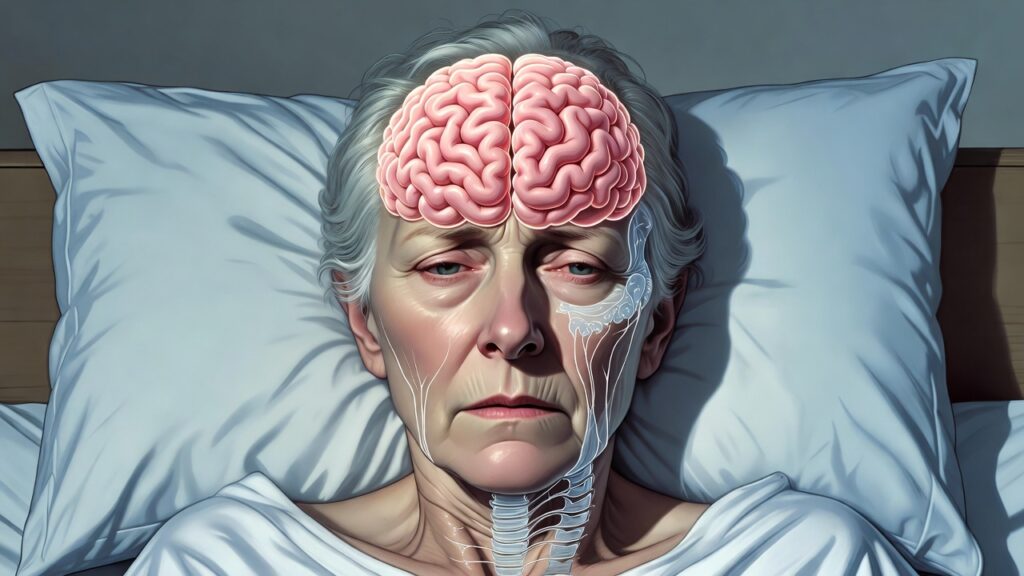
Nipah virus originates in animals and can be passed to humans through direct or indirect contact. It is classified under the Paramyxoviridae family and belongs to the Henipavirus genus, which also includes the equally lethal Hendra virus. Unlike many common viral infections, Nipah virus demonstrates a strong tendency to attack both the central nervous system and the respiratory system. This often leads to acute brain inflammation (encephalitis), serious breathing difficulties, and a high risk of mortality.
• A high rate of case fatalities
•Signs in the brain and mental health.
There are no specific vaccines or treatments for viruses
Origin and Discovery of Nipah Virus

The Nipah virus was first discovered during a Malaysian outbreak in 1998–1999. At first, patients, mostly pig farmers, presented with neurological symptoms, altered consciousness, and fever. The initial diagnosis of these cases as Japanese encephalitis was incorrect. Further epidemiological and virological investigations revealed that:
• Fruit bats, particularly those belonging to the genus Pteropus, served as the virus’s natural reservoir.
•The virus was transmitted from bats to pigs
• After infecting pigs, the virus spread to humans.
The virus was named Nipah virus after Sungai Nipah, the village where the outbreak was first recognized.
Human-to-human transmission, especially among family members and healthcare workers, emerged as a significant and alarming feature in subsequent outbreaks in Bangladesh and India.
Natural Reservoir and Transmission Pathways

Fruit Bats as the Natural Host
Nipah virus is carried asymptomatically by fruit bats. They spread the virus by:
- Urine
- Blood
- Feces
The virus can contaminate food sources and surfaces without causing illness in the bats themselves.
Modes of Transmission

- Animal-to-Human Transmission
o Contact with infected pigs or other animals
o Working with sick animals without protective gear
- Foodborne Transmission
o Consumption of bat-contaminated raw date palm sap
o Eating fruits partially eaten or contaminated by bats
- Human-to-Human Transmission
o Indirect contact with infected individuals’ bodily fluids o Droplets that are exhaled
o Close caregiving contact
o Poor infection control in healthcare settings
The Nipah virus’s capacity for person-to-person transmission significantly increases its potential for pandemic.
Incubation Period
In rare instances, longer incubation periods of up to 45 days have been reported. The typical incubation period is between four and fourteen days. Early detection and containment are made more difficult by this variability.
Clinical Manifestations of Nipah Virus Infection
Early Symptoms
Initial symptoms are often nonspecific and resemble common viral illnesses, which can delay diagnosis:
- Fever
- Headache
- Myalgia
- Fatigue
- Nausea and vomiting
Progressive Symptoms
Patients may develop the following as the disease progresses:
- Persistent cough
- Shortness of breath
- Sore throat
- Dizziness
- Altered mental status
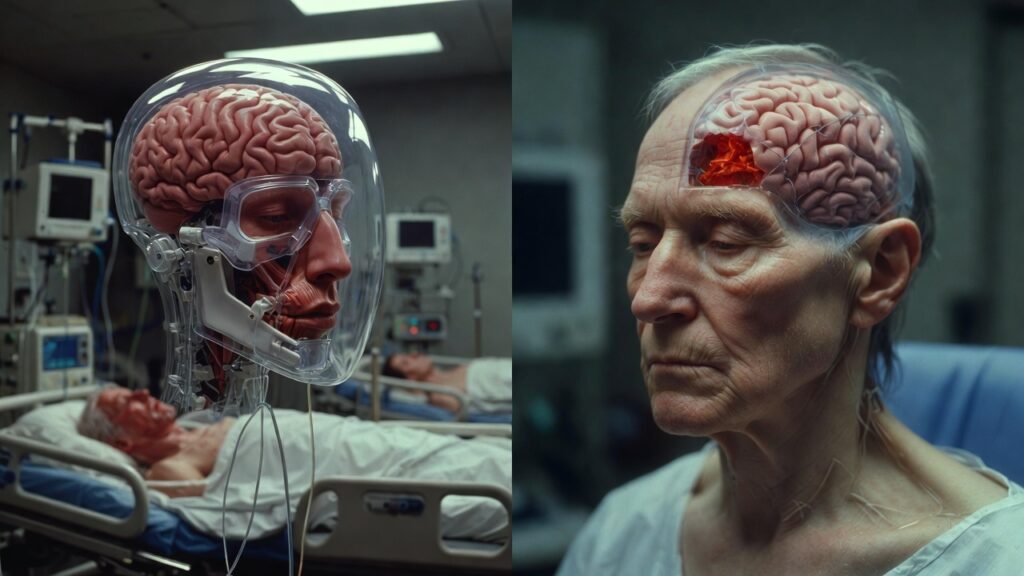
Severe and Life-Threatening Symptoms
In severe cases, Nipah virus causes:
- Acute encephalitis
- Seizures
- Loss of consciousness
- Coma
- Acute respiratory failure
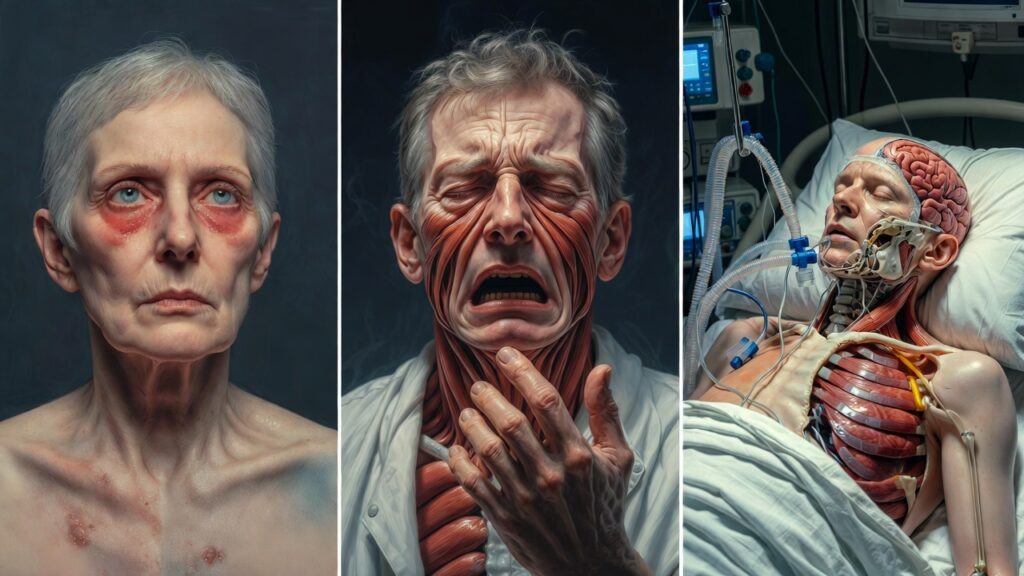
Neuropsychiatric Manifestations
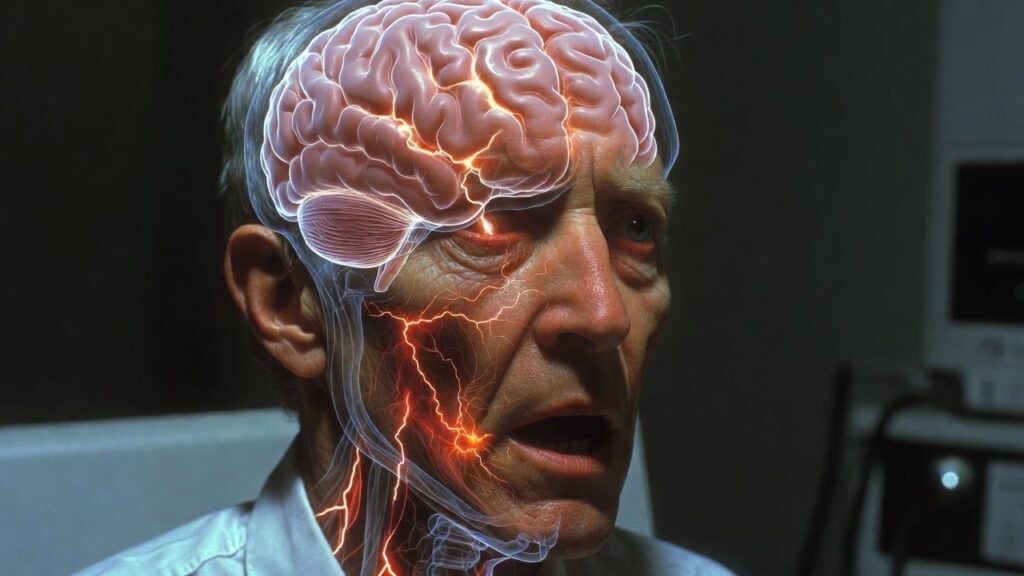
The Nipah virus is particularly troubling from a neurological and psychiatric point of view. In my clinical perspective, patients may exhibit:
• Acute delirium and confusion
• Behavior deprivation
• Anxiety and agitation
• Hallucinations
• Personality development
These symptoms emphasize the virus’s direct brain involvement and emphasize the need for multidisciplinary care.
Complications and Long-Term Consequences
High Mortality Rate
The nipah virus infection rate can range anywhere from 40% to 75%, depending on the outbreak and the healthcare infrastructure that is in place.
Neurological Sequelae in Survivors
Survivors may suffer from long-term complications, including:
- Persistent cognitive impairment
- Memory deficits
- Speech and motor difficulties
- Seizure disorders
- Chronic fatigue
Psychiatric and Psychological Impact
Although prevalent, post-infection psychiatric disorders are frequently overlooked:
• Irritation
• Anxiety disorders
• Post-traumatic stress disorder (PTSD)
• Social withdrawal
These conditions have a significant impact on quality of life and necessitate ongoing mental health care.
Diagnosis of Nipah Virus

A high suspicion level and specialized laboratory facilities are required for diagnosis. Common diagnostic methods include:
• RT-PCR testing of blood, cerebrospinal fluid, urine, or throat swabs
• ELISA for antibody detection
Early diagnosis is critical but challenging, particularly in low-resource settings.
Treatment and Clinical Management

Lack of Specific Treatment
There is neither a vaccine nor an approved treatment for the Nipah virus at this time.
Supportive Care
- Management is largely supportive and includes:
- Intensive care monitoring
- Treatment with oxygen or mechanical ventilation
- Management of seizures
- Management of cerebral edema
- Strict isolation precautions
Experimental Therapies
Ribavirin, for instance, has been the subject of research with mixed results. Although currently under investigation, monoclonal antibodies and vaccine candidates are not widely available.
Prevention and Infection Control

Given the absence of definitive treatment, prevention remains the most effective strategy.
Public Health Measures
-
Avoid consumption of raw date palm sap
-
Clean fruits by peeling them before eating them.
-
Prevent bats from accessing food sources
Healthcare Precautions
-
Wearing personal protective gear (PPE)
-
Stringent methods for preventing infections
-
Isolation of suspected cases
Psychological and Social Dimensions
From a mental health perspective, Nipah virus outbreaks frequently result in:
• Fear and panic
• Negative perceptions of patients and their families
• Rumors and erroneous information
To prevent long-term harm to society, mental health interventions must be incorporated into outbreak response plans.
Global Health Significance

The Nipah virus is deemed a priority pathogen by the World Health Organization because of:
• The high death rate
• Pandemic potential
• A lack of options for treatment
In an increasingly interconnected world, emerging infections like Nipah virus underscore the urgent need for global surveillance, research collaboration, and preparedness.
Conclusion
One of the most significant new infectious threats of the modern era is the nipah virus. Its ability to cause devastating neurological disease, combined with high mortality and limited treatment options, demands urgent attention from clinicians, researchers, and policymakers alike.
The fight against the Nipah virus requires more than just medical treatment, according to my clinical experience and a review of the most recent scientific evidence. It necessitates:
- Early detection
- Public education
- Reliable health care systems
- Integration of mental health care
- Cooperation across borders
Only through a comprehensive and proactive approach can we hope to mitigate the devastating impact of this silent but deadly virus.

